Clinical Study
Precision Diagnostics: Protecting Patients Now and for the Future
Steven Goldberg, MD, MBA • Feb 3, 2026
Urgent care providers are on the frontlines of the fight against antimicrobial resistance, and next-morning PCR testing gives them the tools to win.
Introduction
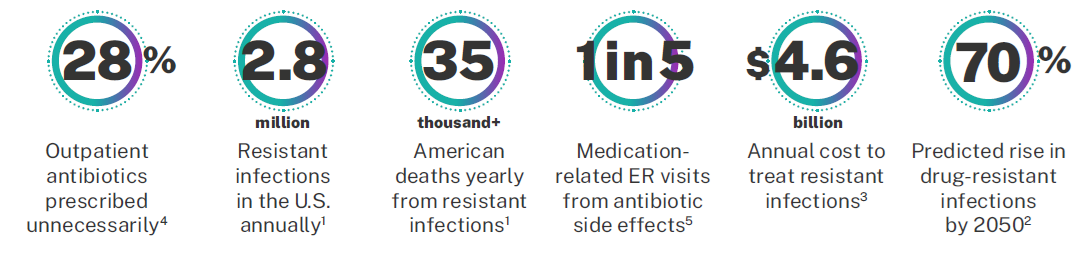
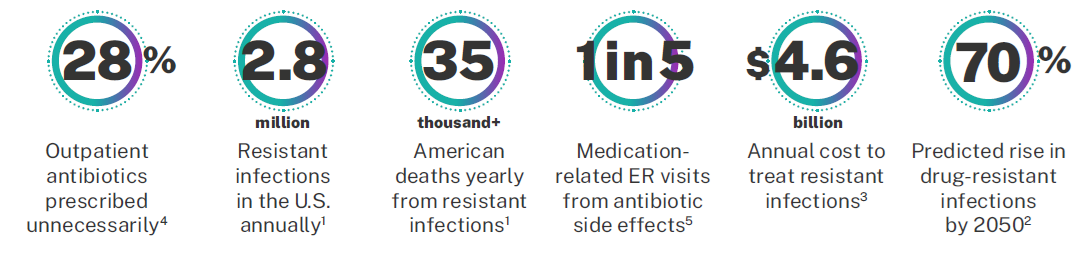
Antimicrobial resistance (AMR) represents one of the most urgent public health threats facing communities worldwide. With 2.8 million resistant infections occurring in the U.S. annually and over 35,000 Americans dying each year from these infections, the stakes have never been higher.1 By 2050, drug-resistant infections are predicted to rise by 70%, leading to 40 million deaths globally and 2 million in the U.S. each year.2 The economic burden is equally staggering, with an estimated $4.6 billion spent annually to treat Americans with antimicrobial-resistant infections.3
The Urgent Care Dilemma: Speed vs. Precision
Urgent care providers face a unique challenge in the battle against AMR. Patients arrive expecting fast answers and immediate relief. Traditional diagnostic methods take days to deliver results; time that symptomatic patients simply don’t have. This pressure creates a clinical catch-22: empirically prescribing antibiotics “just in case” to meet patient expectations, or waiting for test results while symptoms persist.
The consequences of this waiting game are significant. Up to 28% of outpatient antibiotics are prescribed unnecessarily,4 and 1 in 5 medication-related emergency room visits stem from antibiotic side effects.5 When providers lack diagnostic certainty, they often default to broad-spectrum antibiotics—a practice that accelerates resistance development and exposes patients to unnecessary risks.
This approach has become normalized in urgent care settings, where high patient volumes and time constraints discourage testing altogether. The result? A self-perpetuating cycle where lack of testing leads to overprescription, which fuels resistance, which leads to more complicated infections, which increases costs and poorer outcomes for everyone.
By The Numbers: The Cost of Uncertainty
Breaking the Cycle: Precision Diagnostics as the Solution
What if urgent care providers could deliver both speed and precision? Next-morning PCR testing for infectious disease changes the equation entirely. HealthTrackRx has pioneered a nationwide diagnostic model that gives providers molecular-level answers by the next morning. That’s fast enough to meet patient expectations while precise enough to support evidence-based prescribing.
This isn’t an incremental improvement. It’s a fundamental shift in how urgent care can approach infectious disease. Samples collected are processed overnight, with results available when providers open their doors the next morning. This turnaround enables targeted treatment decisions within a clinically relevant timeframe.
The impact extends beyond individual patient encounters. PCR testing identifies pathogens and resistance genes that cultures often miss, allowing providers to prescribe the right antibiotic at the right dose or avoid antibiotics entirely when infections prove viral. This precision reduces unnecessary broad-spectrum prescribing, minimizes antibiotic exposure, and slows the development of resistance.
By the Numbers: The Savings with Precision
The clinical and economic benefits are measurable. Urgent care providers using next-morning PCR testing reported:

For respiratory and pharyngitis cases alone, PCR testing demonstrates 3 fewer outpatient visits per 6 months and $370 in cost avoidance per patient compared to traditional culture testing.7
Perhaps most importantly, 98% of providers report improved patient outcomes6—proof that speed and precision aren’t opposing forces but complementary goals. Patients receive confident diagnoses and appropriate treatment plans without the anxiety of waiting days for answers or the risks of unnecessary medications.
The Path Forward: Antibiotic Stewardship at Scale
Every prescription decision made in urgent care ripples outward, affecting community resistance patterns and population health. Next-morning PCR testing empowers providers to be active participants in antibiotic stewardship. Plus, this is achieved without added complexity or workflow disruption by delivering better information when it matters most.
The technology exists. The infrastructure is proven. What’s needed now is widespread adoption of diagnostic approaches that meet the unique demands of the urgent care environment. Embracing precision diagnostics allows urgent care providers to continue delivering the fast, convenient care patients expect, while also protecting the effectiveness of antibiotics for future generations.
The choice is clear: we can continue the status quo or make a change for the better. For the sake of our patients, our communities, and public health, it’s time to choose precision.
References
- Centers for Disease Control and Prevention. (2025). Antimicrobial resistance: Causes and how it spreads.
- Nature. 40 million deaths by 2050: Toll of drug-resistant infections to rise by 70%.
- Nelson, R. E., Hatfield, K. M., Wolford, H., et al. (2021). National estimates of healthcare costs associated with multidrug-resistant bacterial infections among hospitalized patients in the United States. Clinical Infectious Diseases, 72(Suppl 1), S17–S26.
- Hersh, A. L., King, L. M., Shapiro, D. J., Hicks, L. A., & Fleming-Dutra, K. E. (2021). Unnecessary antibiotic prescribing in US ambulatory care settings, 2010–2015. Clinical Infectious Diseases, 72(1), 133–137.
- Shehab, N., Lovegrove, M. C., Geller, A. I., et al. (2016). US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA, 316(20), 2115–2125.
- Alexander, B. A., et al. (2025). Pathogen molecular testing and its impact on antibiotic prescribing and patient outcomes: Results of a provider survey. Journal. (In review).
- Evans, et al. (2025). Healthcare resource utilization and costs among patients receiving diagnostic tests for respiratory infections. American Journal of Managed Care.
References
- Centers for Disease Control and Prevention. (2025). Antimicrobial resistance: Causes and how it spreads.
- Nature. 40 million deaths by 2050: Toll of drug-resistant infections to rise by 70%.
- Nelson, R. E., Hatfield, K. M., Wolford, H., et al. (2021). National estimates of healthcare costs associated with multidrug-resistant bacterial infections among hospitalized patients in the United States. Clinical Infectious Diseases, 72(Suppl 1), S17–S26.
- Hersh, A. L., King, L. M., Shapiro, D. J., Hicks, L. A., & Fleming-Dutra, K. E. (2021). Unnecessary antibiotic prescribing in US ambulatory care settings, 2010–2015. Clinical Infectious Diseases, 72(1), 133–137.
- Shehab, N., Lovegrove, M. C., Geller, A. I., et al. (2016). US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA, 316(20), 2115–2125.
- Alexander, B. A., et al. (2025). Pathogen molecular testing and its impact on antibiotic prescribing and patient outcomes: Results of a provider survey. Journal. (In review).
- Evans, et al. (2025). Healthcare resource utilization and costs among patients receiving diagnostic tests for respiratory infections. American Journal of Managed Care.
Related Articles and White papers
Steven Goldberg, MD, MBA • Feb 3, 2026
Urgent care providers are on the frontlines of the fight against antimicrobial resistance, and next-morning PCR testing gives them the tools to win.
Introduction
Antimicrobial resistance (AMR) represents one of the most urgent public health threats facing communities worldwide. With 2.8 million resistant infections occurring in the U.S. annually and over 35,000 Americans dying each year from these infections, the stakes have never been higher.1 By 2050, drug-resistant infections are predicted to rise by 70%, leading to 40 million deaths globally and 2 million in the U.S. each year.2 The economic burden is equally staggering, with an estimated $4.6 billion spent annually to treat Americans with antimicrobial-resistant infections.3
The Urgent Care Dilemma: Speed vs. Precision
Urgent care providers face a unique challenge in the battle against AMR. Patients arrive expecting fast answers and immediate relief. Traditional diagnostic methods take days to deliver results; time that symptomatic patients simply don’t have. This pressure creates a clinical catch-22: empirically prescribing antibiotics “just in case” to meet patient expectations, or waiting for test results while symptoms persist.
The consequences of this waiting game are significant. Up to 28% of outpatient antibiotics are prescribed unnecessarily,4 and 1 in 5 medication-related emergency room visits stem from antibiotic side effects.5 When providers lack diagnostic certainty, they often default to broad-spectrum antibiotics—a practice that accelerates resistance development and exposes patients to unnecessary risks.
This approach has become normalized in urgent care settings, where high patient volumes and time constraints discourage testing altogether. The result? A self-perpetuating cycle where lack of testing leads to overprescription, which fuels resistance, which leads to more complicated infections, which increases costs and poorer outcomes for everyone.
By The Numbers: The Cost of Uncertainty
Breaking the Cycle: Precision Diagnostics as the Solution
What if urgent care providers could deliver both speed and precision? Next-morning PCR testing for infectious disease changes the equation entirely. HealthTrackRx has pioneered a nationwide diagnostic model that gives providers molecular-level answers by the next morning. That’s fast enough to meet patient expectations while precise enough to support evidence-based prescribing.
This isn’t an incremental improvement. It’s a fundamental shift in how urgent care can approach infectious disease. Samples collected are processed overnight, with results available when providers open their doors the next morning. This turnaround enables targeted treatment decisions within a clinically relevant timeframe.
The impact extends beyond individual patient encounters. PCR testing identifies pathogens and resistance genes that cultures often miss, allowing providers to prescribe the right antibiotic at the right dose or avoid antibiotics entirely when infections prove viral. This precision reduces unnecessary broad-spectrum prescribing, minimizes antibiotic exposure, and slows the development of resistance.
By the Numbers: The Savings with Precision
The clinical and economic benefits are measurable. Urgent care providers using next-morning PCR testing reported:

For respiratory and pharyngitis cases alone, PCR testing demonstrates 3 fewer outpatient visits per 6 months and $370 in cost avoidance per patient compared to traditional culture testing.7
Perhaps most importantly, 98% of providers report improved patient outcomes6—proof that speed and precision aren’t opposing forces but complementary goals. Patients receive confident diagnoses and appropriate treatment plans without the anxiety of waiting days for answers or the risks of unnecessary medications.
The Path Forward: Antibiotic Stewardship at Scale
Every prescription decision made in urgent care ripples outward, affecting community resistance patterns and population health. Next-morning PCR testing empowers providers to be active participants in antibiotic stewardship. Plus, this is achieved without added complexity or workflow disruption by delivering better information when it matters most.
The technology exists. The infrastructure is proven. What’s needed now is widespread adoption of diagnostic approaches that meet the unique demands of the urgent care environment. Embracing precision diagnostics allows urgent care providers to continue delivering the fast, convenient care patients expect, while also protecting the effectiveness of antibiotics for future generations.
The choice is clear: we can continue the status quo or make a change for the better. For the sake of our patients, our communities, and public health, it’s time to choose precision.
References
- Centers for Disease Control and Prevention. (2025). Antimicrobial resistance: Causes and how it spreads.
- Nature. 40 million deaths by 2050: Toll of drug-resistant infections to rise by 70%.
- Nelson, R. E., Hatfield, K. M., Wolford, H., et al. (2021). National estimates of healthcare costs associated with multidrug-resistant bacterial infections among hospitalized patients in the United States. Clinical Infectious Diseases, 72(Suppl 1), S17–S26.
- Hersh, A. L., King, L. M., Shapiro, D. J., Hicks, L. A., & Fleming-Dutra, K. E. (2021). Unnecessary antibiotic prescribing in US ambulatory care settings, 2010–2015. Clinical Infectious Diseases, 72(1), 133–137.
- Shehab, N., Lovegrove, M. C., Geller, A. I., et al. (2016). US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA, 316(20), 2115–2125.
- Alexander, B. A., et al. (2025). Pathogen molecular testing and its impact on antibiotic prescribing and patient outcomes: Results of a provider survey. Journal. (In review).
- Evans, et al. (2025). Healthcare resource utilization and costs among patients receiving diagnostic tests for respiratory infections. American Journal of Managed Care.
References
- Centers for Disease Control and Prevention. (2025). Antimicrobial resistance: Causes and how it spreads.
- Nature. 40 million deaths by 2050: Toll of drug-resistant infections to rise by 70%.
- Nelson, R. E., Hatfield, K. M., Wolford, H., et al. (2021). National estimates of healthcare costs associated with multidrug-resistant bacterial infections among hospitalized patients in the United States. Clinical Infectious Diseases, 72(Suppl 1), S17–S26.
- Hersh, A. L., King, L. M., Shapiro, D. J., Hicks, L. A., & Fleming-Dutra, K. E. (2021). Unnecessary antibiotic prescribing in US ambulatory care settings, 2010–2015. Clinical Infectious Diseases, 72(1), 133–137.
- Shehab, N., Lovegrove, M. C., Geller, A. I., et al. (2016). US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA, 316(20), 2115–2125.
- Alexander, B. A., et al. (2025). Pathogen molecular testing and its impact on antibiotic prescribing and patient outcomes: Results of a provider survey. Journal. (In review).
- Evans, et al. (2025). Healthcare resource utilization and costs among patients receiving diagnostic tests for respiratory infections. American Journal of Managed Care.





